Abstract
Introduction
Acute Promyelocytic Leukemia (APL) is the most curable leukemia with reported survival >90% in large co-operative group studies. Induction-related deaths from bleeding, infection, and differentiation syndrome (DS) remain a threat with early death (ED) rate of 30%. DS is a unique and life-threatening complication of APL induction, characterized by unexplained fever, weight gain, pleuropericardial effusion, hypoxemia, hypotension, and/or vascular capillary leak syndrome leading to peripheral edema and acute renal failure. These pathophysiologic complications are sequelae cytokine release from malignant promyelocytes. This clinical diagnosis is without identifying markers. We report our observation on the utility of D-dimer level as a potential marker for the identification of DS, infection and death during APL induction.
Methods
We conducted retrospective chart reviews of APL patients treated at Emory University and co-managed at community and academic treatment centers throughout Georgia, South Carolina and bordering states from 7/2013 to 4/2017 with the purpose of decreasing ED. IRB approval was obtained. Elevations in D-dimer were based on laboratory specific reference values.
Results
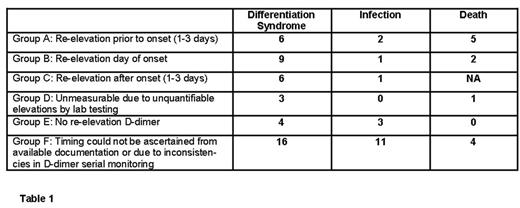
138 patients were enrolled in this study, of whom 44 patients (32%) developed DS and 18 patients (13%) developed infection during induction. We followed the D-dimer trends in those patients that had serial levels obtained throughout induction therapy. At time of presentation, 100% of patients had elevated D-dimer. As disseminated intravascular coagulation (DIC) corrected, there was a drop in D-dimer. D-dimer re-elevated in 6 patients prior to DS onset (14%), 9 patients on day of DS onset (20%), and 6 patients after DS onset (14%). 3 patients (7%) that developed DS had D-dimers that remained elevated at levels unquantifiable by lab testing. 4 patients demonstrated no re-elevation in D-dimer in relation to DS onset (9%). Data was not available to ascertain D-dimer correlation with DS onset in 16 patients (36%). Infection data was collected and patients who developed infection during induction, excluding viral etiologies and pneumonia/pneumonitis due to correlation and overlap with DS presentation, were included totaling 18 patients. Re-elevation of D-dimer was noted in 4 patients in correlation to infection onset (22%), no re-elevation was noted in 3 (17%), and data was not available in 11 patients (61%). 12 patients died due to induction-related complications. D-dimer was re-elevated in relation to timing of death in 7 patients (58%), remained unmeasurably high in 1 (8%), and data was not available in 4 patients (33%). Table 1.
Conclusion
D-Dimer is a marker of inflammation and is elevated in inflammatory processes. Most patients presenting with APL have high D-dimer levels secondary to DIC. A repeat elevation after an initial decrease might be a useful marker of foreboding complications in APL, including DS, infection, and death. As evidenced in our study, there remain a significant number of patients with inconsistencies in D-dimer serial monitoring or entire lack thereof. Given the impressive correlation between D-dimer and aforementioned complications that our review demonstrates, this supports incorporating D-dimer in daily lab monitoring as a standard of care. Our observations, if confirmed in larger studies, could be a valuable addition to identifying induction-related complications earlier and decreasing incidence of early deaths.
Arellano: Cephalon Oncology: Research Funding. Kota: Xcenda: Consultancy; Leukemia Lymphoma Society: Research Funding; Takeda Pharmaceuticals: Consultancy; Incyte: Consultancy; Novartis: Consultancy; Pfizer: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal